Melanoma Research Group
Melanoma is the sixth most common cancer in Scotland. It arises when the cells in the body that produce pigment, melanocytes, undergo changes that enable them to first undergo a large number of replications and then to spread to other parts of the body.
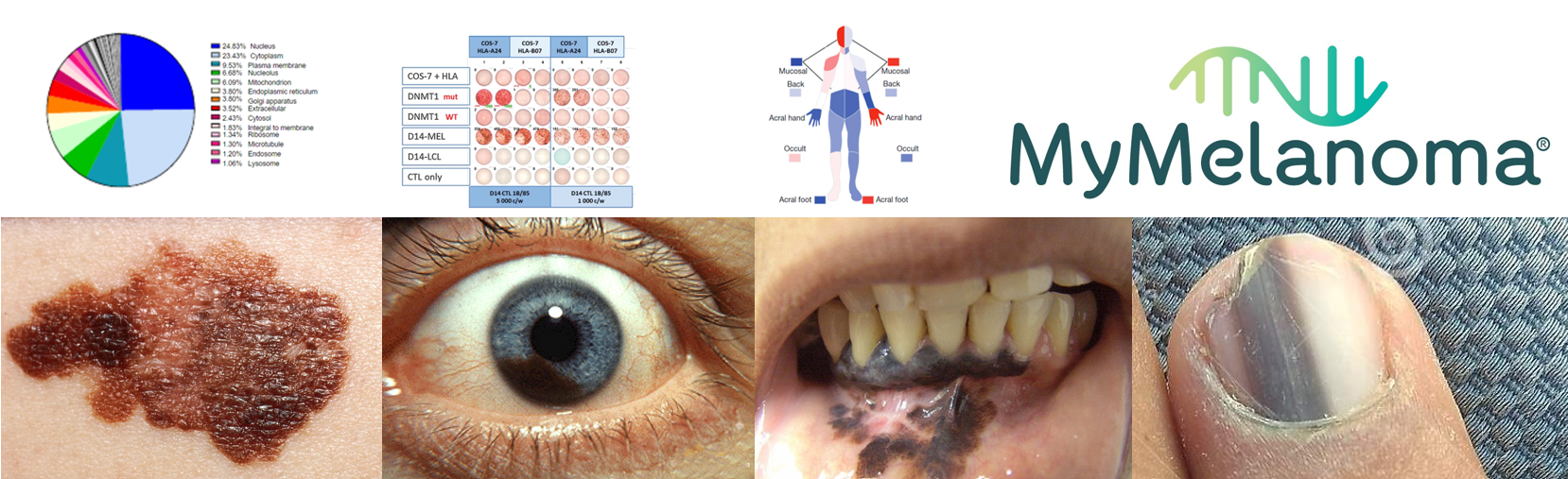
Melanoma can occur in four main locations in the body:
- non-glabrous skin, known as cutaneous melanoma
- glabrous skin (soles of the feet, palms of the hands, under the nail), known as acral melanoma
- the uveal tract of the eye, known as uveal melanoma
- the mucosa of the body (such as the mouth, nose, genital tract), known as mucosal melanoma
When detected early, melanoma has an excellent prognosis. Unfortunately, once melanoma has spread, it is one of the hardest cancers to cure. The main goals of our research are therefore focused on ways to better identify people at greater risk of developing melanoma and to find better ways to treat the melanoma once it has spread.
Contact the team at melanoma.research@uhi.ac.uk
Research Team
Associate Professor Antonia Pritchard
A/Prof. Pritchard formed the Cancer Research Group in 2017. It has since then focused notably on melanoma.
Research Biography and Publications
Dr Colette Mustard
Inspirational former team members
Dr Sharon Hutchison (3 April 1908 - 28 December 2019) was a senior post-doctoral researcher within the Cancer Research Group. In January 2019, she noticed new changes to a mole on her neck, which was diagnosed as a cutaneous melanoma. Sadly only a few months later, it had spread to her lymph nodes and lung. Despite getting the best possible treatment available, it spread further and we said our final goodbye at the end of December 2019.
Sharon was an excellent researcher, who passionately worked towards improving outcomes for people who develop melanoma in the years before her own diagnosis. Her loss, both personally to us and to the wider research community, is immeasurable and we miss her every day. Sharon’s experiences during her melanoma treatment have re-shaped our approach to our research and the kind of work we are carrying out. We have been forever affected by losing Sharon and as a result, are more driven than ever to find new ways to prevent and treat this terrible disease.
Our Major Collaborators
Our Major Collaborators
- Nick Hayward: https://www.qimrberghofer.edu.au/people/nicholas-hayward/
- Peter Johansson: https://www.qimrberghofer.edu.au/people/peter-johansson/
- GenoMEL - https://genomel.org/
- Julia Newton-Bishop - https://medicinehealth.leeds.ac.uk/medicine/staff/648/professor-julia-newton-bishop
- David Adams: https://www.sanger.ac.uk/person/adams-david/
- Kevin Brown: https://irp.nih.gov/pi/kevin-brown
- Anna Bibby: https://research-information.bris.ac.uk/en/persons/anna-c-bibby
- Rona MacKie: https://en.wikipedia.org/wiki/Rona_MacKie
MyMelanoma
MyMelanoma
MyMelanoma is a one-of-a-kind collaborative research project working with melanoma sufferers to facilitate the most ambitious melanoma patient study ever conducted.
MyMelanoma aims to develop the first digital platform for melanoma research, collating data derived from a patient-centred collaboration with researchers, medical staff and scientists, to enable better care and cure in the next ten years.
A/Prof. Pritchard is the lead researcher at UHI for the MyMelanoma project focused on the genetic predisposition to melanoma development.
Patient recruitment is now open via the MyMelanoma website.

Genetic predisposition to melanoma
Genetic predisposition to melanoma
Some people are at greater risk of developing melanoma due to alterations in their genetics (DNA). Several genes have been identified as being important in the increased predisposition to melanoma when they contain changes, known as ‘variants’ or ‘mutations’ that change their normal functions.
Some families have a highly increased likelihood of developing melanoma due to mutations in specific genes. These include CDKN2A, CDK4, BAP1, TERT, POT1, ACD and TERF2IP. Mutations to some of these genes also increase the predisposition to some other cancers, such as pancreatic, mesothelioma, glioma, chronic lymphocytic leukaemia and clear cell renal cell carcinoma, in these families.


Other genes cause an increased predisposition to melanoma development when they are changed, to a lower degree than the familial genes. These include genes that alter pigmentation, controlling skin, eye and hair colour, as well as those controlling repair to DNA damage.
Our studies in this area aim:
- To better understand the risk to cancer development when people carry mutations in genes already known to increase predisposition to all types of melanoma and other cancers. We are aiming to improve the advice and screening regime given to patients carrying these variants.
- To identify the genetic mutations present in people with increased risk to all types of melanoma, but do not have mutations present in these known genes.


-99x60.jpg)
-100x70.jpg)
If you are interested in taking part in this project, please email antonia.pritchard@uhi.ac.uk
Immune response to melanoma
Immune response to melanoma
The immune system of the body is capable of identifying and killing cancer cells. This has been harnessed for the treatment of cutaneous melanoma, in a type of drug called ‘immunotherapy’. These therapies target a specialised kind of immune cell, to reinvigorate the immune response against the tumours. Despite revolutionising the treatment of cutaneous melanoma, there are still a large number of patients who do not respond, or develop resistance to, the therapy. Furthermore, these treatments frequently do not work well against the other types of melanoma.
Our research is aiming to better understand the immune response to melanomas.

If you currently have a melanoma and are interested in taking part in this project, please email for further details: antonia.pritchard@uhi.ac.uk